News
Cancer Rehabilitation Awareness Week 2024
Cancer rehabilitation is focused on improving the quality of life and experience of people who have been diagnosed with cancer. It is not focused on the disease, it is focused on people, and helping them get back to living. The unseen struggles Cancer survival rates have dramatically increased in the past forty years as a…
Read MoreWhat is DeQuervain’s Tenosynovitis?
Description DeQuervain’s Tenosynovitis, common in office workers, new parents, and jobs requiring repeated thumb and wrist movements, is a condition whereby the tendons of the thumb side of the wrist become inflamed from an increase in repetitive wrist and thumb movements. Pain generally occurs upon movement of the wrist and thumb. There can also be…
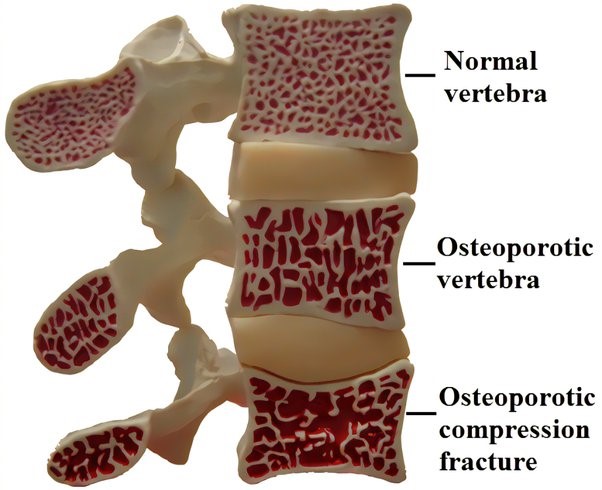
Read MoreAll You Need To Know About Osteoporosis And How To Keep Your Bones Strong
Osteoporosis is a condition where bones lose important minerals such as calcium quicker than they can be replaced by the body, resulting in a decrease in the thickness or density of bones. This can lead to them becoming fragile & brittle, and at a higher risk of fractures than normal bone. Often called the “silent…
Read MoreWhat To Know About Soccer Pre-Season Training
The three main phases of training for athletes in their chosen sport are pre-season, in-season, and off-season. Pre-season training is a phase of training that athletes complete before the commencement of their season for their chosen sport, mainly focusing on preparing for the competition by developing the fundamentals required for their sport. Professional soccer athletes…
Read MoreDoes Physiotherapy Help Frozen Shoulder?
Frozen shoulder is characterised by a painful and stiff shoulder. The lining (capsule) of the shoulder becomes inflamed and stiff, causing shooting pain with certain arm movements such as lifting the arm. In most cases, frozen shoulder symptoms come on gradually however, a frozen shoulder can also come on without warning. Generally, it starts with…
Read More5 FRIENDLY EXERCISE TIPS TO GET MOVING & STAY MOVING OVER CHRISTMAS
With Christmas and the holiday season drawing near, it becomes much harder to stick to regular exercise routines. Here are a few friendly tips to help get moving and stay moving over the Christmas break. Just remember any exercise is better than no exercise! Exercise – Think short & effective Shorter periods of exercise,…
Read MoreWe are looking for a full or part-time physio!
Description We have an exciting opportunity for a junior or experienced Physiotherapist to join our team. Commencing immediately and working on a full or part time basis, the role will involve supporting our busy schedule Physio-led Exercise (clinical pilates) classes plus in rooms physiotherapy. At Inner Strength Bayside Physiotherapy we all have an interest in Physio-led Exercise, drawing…
Read MoreIntroducing Glow Acupuncture to Inner Strength Bayside!
Jessica Minogue, from Glow Acupuncture, is an AHPRA registered Chinese Medicine practitioner, consulting from the rooms at Inner Strength Bayside on Tuesdays, Thursdays, Fridays & Saturdays. She offers Acupuncture, Chinese herbal medicine, cupping and cosmetic acupuncture. Interested in Chinese Medicine but don’t really understand how it works? Chinese medicine works on evaluating health conditions holistically.…
Read More3 Must-Do Exercises For Every Cricketer
Cricket is a popular sport in Australia and has a reputation of being a “slow paced” game, it is now becoming faster and more dynamic which leaves cricket players open to a fair share of injuries! Professional cricketers are now extremely fit, strong and athletic and as the saying goes “Prevention is better than cure!” Try and do these exercises 3x…
Read MoreSore Feet?
Are your feet a little sore as the weather warms up and you adjust to a change in footwear? You may have pain in the heel, toes, arch, instep, or insole of the foot. Multiple factors may be responsible for producing foot pain such as: increased time spent on your feet with social events etc.,…
Read More