Leaders in Physiotherapy and Physio-led Exercise
News
Cancer Rehabilitation Awareness Week 2024
Cancer rehabilitation is focused on improving the quality of life and experience of people who have been diagnosed with cancer. It is not focused on the disease, it is focused on people, and helping them get back to living. The unseen struggles Cancer survival rates have dramatically increased in the past forty years as a result of improvements in cancer…
Read MoreUnderstanding Your Clinical Pilates Exercise Program: The Reason Behind Why You May Be Only Exercising On One Side Of Your Body.
Do you notice that all your injuries occur on one side of your body? That you may feel like you have one side that is a lot weaker/more injury prone than the other? Or that exercises in standing vs sitting are more effective? Re-occurrent injuries on one side of the body is something that we often see as physiotherapists and…
Read MoreWhat Is An Abdominal Muscle Separation Post Child Birth (DRAM)?
What is a DRAM? Diastasis Rectus Abdominis Muscle (DRAM) is the stretching of the two rectus abdominus muscles at the midline, also known as the linea alba. This is a healthy body’s normal physiological change, which occurs typically during the second and third trimester of pregnancy as the body allows room for the baby to grow. What Causes DRAM?…
Read MoreWhat is DeQuervain’s Tenosynovitis?
Description DeQuervain’s Tenosynovitis, common in office workers, new parents, and jobs requiring repeated thumb and wrist movements, is a condition whereby the tendons of the thumb side of the wrist become inflamed from an increase in repetitive wrist and thumb movements. Pain generally occurs upon movement of the wrist and thumb. There can also be thickening and swelling around the…
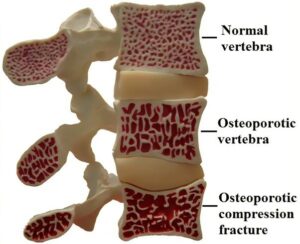
Read MoreAll You Need To Know About Osteoporosis And How To Keep Your Bones Strong
Osteoporosis is a condition where bones lose important minerals such as calcium quicker than they can be replaced by the body, resulting in a decrease in the thickness or density of bones. This can lead to them becoming fragile & brittle, and at a higher risk of fractures than normal bone. Often called the “silent disease”, osteoporosis can occur without…
Read MoreWhat To Know About Soccer Pre-Season Training
The three main phases of training for athletes in their chosen sport are pre-season, in-season, and off-season. Pre-season training is a phase of training that athletes complete before the commencement of their season for their chosen sport, mainly focusing on preparing for the competition by developing the fundamentals required for their sport. Professional soccer athletes commencing their pre-season training, use…
Read MoreDoes Physiotherapy Help Frozen Shoulder?
Frozen shoulder is characterised by a painful and stiff shoulder. The lining (capsule) of the shoulder becomes inflamed and stiff, causing shooting pain with certain arm movements such as lifting the arm. In most cases, frozen shoulder symptoms come on gradually however, a frozen shoulder can also come on without warning. Generally, it starts with dull pain around shoulder and…
Read More5 FRIENDLY EXERCISE TIPS TO GET MOVING & STAY MOVING OVER CHRISTMAS
With Christmas and the holiday season drawing near, it becomes much harder to stick to regular exercise routines. Here are a few friendly tips to help get moving and stay moving over the Christmas break. Just remember any exercise is better than no exercise! Exercise – Think short & effective Shorter periods of exercise, higher intensity Ways to do…
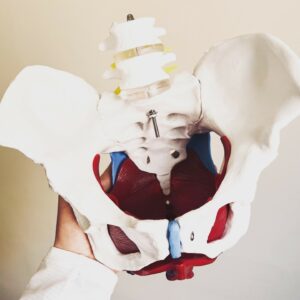
Read MoreWomens Pelvic Health at Inner Strength Bayside
There are a multitude of issues that can occur in and around the pelvis that can cause concern and distress. Pregnancy related concerns, pelvic pain, urinary incontinence, bowel concerns, pelvic organ prolapse, pelvic floor weakness and pelvic pain can all have a significant impact on our quality of life. At Inner Strength Bayside we offer pelvic health services to address…
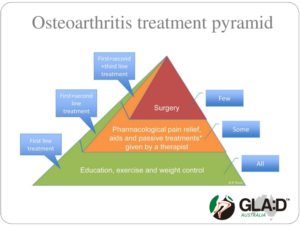
Read MoreGLA:D® – an education and exercise program for people with hip or knee osteoarthritis.
GLA:D®, Good Life with osteoArthritis: Denmark, is an education and exercise program developed by researchers in Denmark for people with hip or knee osteoarthritis symptoms. GLA:D® Australia is a not-for-profit initiative led by La Trobe University. Research from the GLA:D® program in Australia shows: an average pain reduction of 36% reduced pain killers’ consumption reduced expected need for surgery substantial…
Read MoreTIPS TO STICK TO YOUR EXERCISE REGIME
We all have been told about the benefits of exercise for improving mental health, losing weight, improving glucose metabolism and keeping our bones healthy. But how many of us have actually stick to doing regular exercises? Sometimes, it is because we try to fit into someone else’s shoes or follow a recipe which may not work for us!! There are…
Read MoreDiabetes and Physiotherapy
Diabetes is a metabolic disorder in which the body is impaired in regulating sugar levels, specifically glucose, in the blood, either by poor sensitivity to the protein insulin, or due to inadequate production of insulin by the pancreas. As per the International Diabetes Federation (IDF), approximately 415 million adults between the ages of 20 to 79 years had diabetes mellitus in 2015.With unhealthy…
Read More